The Royal Commission into Aged Care report, entitled Care, Dignity and Respect – made public on 1 March – has recommended a major expansion of the aged care and disability workforce.
According to Grattan Institute experts, improved workforce conditions and capability sits as one of the “top four takeaways from this landmark report,” along with the need for a rights-based aged-care system, stronger governance systems for providers and that “a better system will cost more”.
In response to the Royal Commission, the Commonwealth Government immediately committed additional funding of $452.2 million to address immediate priorities, which includes an investment of $92 million to create more than 18,000 places for workers between now and mid-2023. “There will be a significant increase in activity to attract job seekers into the sector, and a new Home Care Workforce Support Program will provide additional targeted support, including assistance to employers to access support and training for new recruits,” Minister Greg Hunt said.
The size of workforce expansion come is enormous, as Bernard Keane writes (Crikey, 5 March 2021, $): "Despite extensive understaffing in the sector, the aged care workforce is already large: 366,000 paid staff, 68,000 volunteers, 28,000 contractors — around 3% of the entire workforce. And it’s going to expand rapidly in coming years. Simply to maintain current (wholly inadequate) staffing levels, the equivalent of an extra 130,000 full time staff will be required in the next 29 years. The commissioners want an additional 80,000 workers by 2030 and an extra 180,000 by 2050 in order to properly staff the sector."
Other issues raised include the importance of aged care provider governance, one of the five pillars of the Government’s “five year roadmap”: $30 million will fund training for an expected 3,700 individuals in governance programs.
Comment by Community Colleges Australia (CCA)
“Australia’s not-for-profit adult and community education providers constitute a major source of qualified aged and disability care professionals, particularly at Certificate III and IV, with almost every CCA member offering these qualifications. Our members have done an excellent job at working closely with aged care providers and we produce qualified, skilled and highly regarded workers. CCA will be most pleased to see the status of aged care workers raised because of this report. We do note, however, that significant worker recruitment may soon take place, and we want to make certain that the quality of this training remains high,” said Dr Don Perlgut, CCA CEO.
"The Royal Commission recommends that there be a mandatory minimum qualification of a Certificate III and minimum levels of English language proficiency; see recommendation 77. Australia's not-for-profit community education providers are the best-situated to provide this training," said Dr Perlgut.
“We are also not surprised that the Aged Care Commissioners have singled out governance. Our experience in vocational education and training is that proper governance – which includes executive leadership – and sufficient funding are the two essentials to make services work,” said Dr Perlgut.
“Our concerns are that these cannot be one-off efforts. Workforce planning and continued governance are essential, not just now but into the future,” said Dr Perlgut.
Additional Background on the Report
The Government’s workforce response reads: “This measure will build on the existing workforce, by ensuring there are sufficient opportunities for workers to gain the necessary skills and training to work in aged care, with a focus on home based care. The measure will seek to attract over 18,000 jobseekers through existing programs (jobactive, Australian Apprenticeships, Job Trainer, Youth Jobs PaTH, and Launch into Work) and the newly established Home and Residential Aged Care Workforce Support Program.”
The report reads: “Care workers are properly valued: Most of the money spent in aged care is spent on the workforce. More needs to be spent to deliver better quality and safe aged care. Aged care is a worthy profession, and it needs to be appreciated as the key means to keep the aged care system safe and of high quality. A sufficient, committed and high quality workforce is one of the main factors affecting the quality and safety of aged care. If an aged care worker is well educated and trained, has the right attitude of respect towards older people and their supportive caring work, and is increasingly experienced, older people will receive better care.” (Volume 1, pp. 40-41)
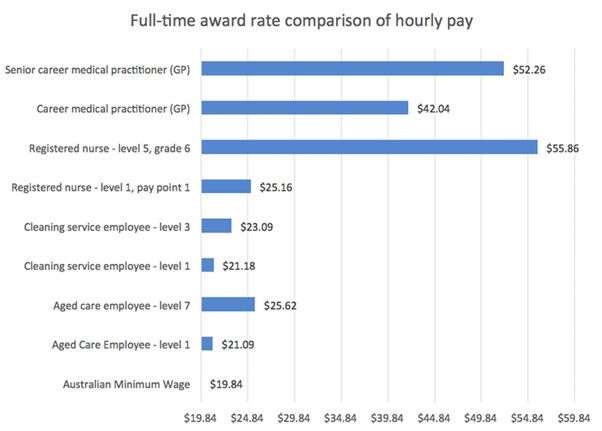
An article in The Conversation (25 February 2021). entitled “Paid on par with cleaners: the broader issue affecting the quality of aged care,” details how poorly some aged care workers are paid – see below:
Other Commentary
Australians support an expanded aged care workforce: “The vast majority of our respondents (86%) either ‘strongly agreed’ or ‘agreed’ Australia needed more skilled and trained aged care workers. On top of this, 80% thought aged care workers should be paid more for the work that they did. More than 80% also either ‘strongly agreed’ or ‘agreed’ that nurses working in aged care should be paid at an equivalent rate to nurses working in the health system. Currently, nurses working in aged care are paid, on average, about 10-15% less,” reported Rachel Milte and Julie Ratcliffe from Flinders University.
Not all observers are optimistic about what the results of the Royal Commission will be. Ross Gittins, in The Sydney Morning Herald, writes “we’re stuck with crappy aged care because Morrison won’t ask the young or the old to pay to fix it…. Implementing the commission’s report would cost a minimum of $10 billion a year and probably a lot more. It’s impossible to imagine this government having the courage to raise anything like that much by tightening the means-testing of its own well-off supporters.”
Patricia Sparrow, CEO of Aged & Community Services Australia, says: “Royal commission research showed that Australia spends around 1.2% of its GDP on aged care, but other comparable countries in the OECD, the average they spend is around 2.5%.... It gives us a sense of the scale and the scope of what’s going to need to be considered. [The Government] will do a serious response, but [there have been] 20 reports over 20 years and that hasn’t happened.”
Michelle Grattan writes: “Aged care is a federal government responsibility and the pandemic exposed the vulnerabilities in the system, with the majority of COVID-19 deaths occurring among aged care residents.”
THE RECOMMENDATIONS
Chapter 12, on the “Aged Care Workforce”, contains the following recommendations:
Recommendation 77: National registration scheme: By 1 July 2022, the Australian Government should establish a national registration scheme for the personal care workforce with the following key features:
- a mandatory minimum qualification of a Certificate III
- ongoing training requirements
- minimum levels of English language proficiency
- criminal history screening requirements
- a code of conduct and power for a registering body to investigate complaints into breaches of the Code of Conduct and take appropriate disciplinary action.
- For existing personal care workers who do not meet the minimum qualification requirements, there should be transitional arrangements that allow them to apply for registration based on their experience and prior learning.
Recommendation 78: Mandatory minimum qualification for personal care workers A Certificate III should be the mandatory minimum qualification required for personal care workers performing paid work in aged care. If a Personal Care Worker National Board is established, it should establish an accreditation authority to develop and review accreditation standards for the mandatory minimum qualification assess programs of study and education providers against the standards, and provide advice to the National Board on accreditation functions. The National Board should approve the accredited program of study, and review the need for personal care workers in home care to have specialised skills or competencies.
Recommendation 79: Review of certificate-based courses for aged care: By January 2022, the Aged Care Services Industry Reference Committee, working with the Australian Government Human Services Skills Organisation as required, should: review the need for specialist aged care Certificate III and IV courses, and regularly review the content of the Certificate III and IV courses and consider if any additional units of competency should be included.
Recommendation 80: Dementia and palliative care training for workers: By 1 July 2022, the Australian Government should implement as a condition of approval of aged care providers, that all workers engaged by providers who are involved in direct contact with people seeking or receiving services in the aged care system undertake regular training about dementia care and palliative care.
Recommendation 81: Ongoing professional development of the aged care workforce: From 1 July 2021, the Australian Government and the States and Territories, through the Skills National Cabinet Reform Committee, should fast-track the development by the Australian Industry and Skills Committee of accredited, nationally recognised short courses, skills sets and micro-credentials for the aged care workforce. The courses should be designed to: a. improve opportunities for learning and professional development, and b. upgrade the skills, knowledge and capabilities of the existing workforce.
Recommendation 82: Review of health professions’ undergraduate curricula: In conducting their regular scheduled reviews of accreditation standards, the relevant accreditation authorities should consider any changes to the knowledge, skills and professional attributes of health professionals so that the care needs of older people are met.
Recommendation 83: Funding for teaching aged care programs: By 1 July 2023, the Australian Government should fund teaching aged care programs for delivery to students in both residential aged care and home care settings. The teaching aged care programs should have designated catchment areas and should: a. collaborate with educational institutions and research entities, b. facilitate clinical placements for university and vocational education and training sector students, c. act as a centre of research and training for aged care in a catchment area, d. act as a hub for approved providers in a particular region and support training of aged care workers from surrounding aged care services.
Recommendation 84: Increases in award wages: Employee organisations entitled to represent the industrial interests of aged care employees covered by the Aged Care Award 2010, the Social, Community, Home Care and Disability Services Industry Award 2010 and the Nurses Award 2010 should collaborate with the Australian Government and employers and apply to vary wage rates in those awards to: reflect the work value of aged care employees in accordance with section 158 of the Fair Work Act 2009 (Cth), and/or seek to ensure equal remuneration for men and women workers for work of equal or comparable value in accordance with section 302 of the Fair Work Act 2009 (Cth).
Recommendation 85: Improved remuneration for aged care workers: In setting prices for aged care, the Pricing Authority should take into account the need to deliver high quality and safe care, and the need to attract sufficient staff with the appropriate skills to the sector, noting that relative remuneration levels are an important driver of employment choice.
Recommendation 86: Minimum staff time standard for residential care: The Australian Government should require approved providers of residential aged care facilities to meet a minimum staff time quality and safety standard. This requirement should take the form of a quality and safety standard for residential aged care. The minimum staff time standard should allow approved providers to select the appropriate skills mix for delivering high quality care in accordance with their model of care. From 1 July 2022, the minimum staff time standard should require approved providers to engage registered nurses, enrolled nurses, and personal care workers for at least 200 minutes per resident per day for the average resident, with at least 40 minutes of that staff time provided by a registered nurse. In addition, from 1 July 2022, the minimum staff time standard should require at least one registered nurse on site per residential aged care facility for the morning and afternoon shifts (16 hours per day). From 1 July 2024, the minimum staff time standard should increase to require approved providers to engage registered nurses, enrolled nurses, and personal care workers for the average resident for at least 215 minutes per resident per day for the average resident, with at least 44 minutes of that staff time provided by a registered nurse. In addition, from 1 July 2024, the minimum staff time standard should require at least one registered nurse on site per residential aged care facility at all times. The minimum staff time standard should be linked to the case mix-adjusted activity based funding model for residential aged care facilities. This means that approved providers with a higher than average proportion of high needs residents would be required to engage additional staff, and vice versa. Approved providers should be able to apply to the System Governor for an exemption from the quality and safety standard relating to staff skills mix, but not the standard relating to numbers of staff. Any exemption should be granted for a limited time, and details of the exemption should be published on My Aged Care. The grounds for granting an exemption should include: a. specific purpose residential aged care facilities, such as specialist homeless facilities, where the profile of the residents is such that it may be appropriate to substitute a registered nurse with another qualified health professional; b. residential aged care facilities that are co-located with a health service, such as Multi-Purpose Services, where registered and enrolled nurses are present at the co-located health service; c. regional, rural and remote residential aged care facilities, where the approved provider can demonstrate it has been unable to recruit sufficient numbers of staff with the requisite skills; and d. residential aged care facilities where an alternative skills mix is being trialled and it would be appropriate to substitute a registered nurse with another qualified health professional. There should be a requirement for any such trial to be comprehensively evaluated and publicly reported. The Australian Commission on Safety and Quality in Health and Aged Care should review and update this standard as appropriate. At a minimum, this should occur in line with significant revisions of the case mix classification for residential aged care facilities, or at least every five years.
Recommendation 87: Employment status and related labour standards as enforceable standards: By 1 January 2022, the Australian Government should require as an ongoing condition of holding an approval to provide aged care services that approved providers: have policies and procedures that preference the direct employment of workers engaged to provide personal care and nursing services on their behalf, where personal care or nursing work is contracted to another entity, that entity has policies and procedures that preference direct employment of workers for work performed under that contract. From 1 January 2022, quality reviews conducted by the Quality Regulator must include assessing compliance with those policies and procedures and record the extent of use of independent contractors.





